SUSS Facts, Tips and Pearls
Massive Transfusion
By Deanna Lee, Stage 1
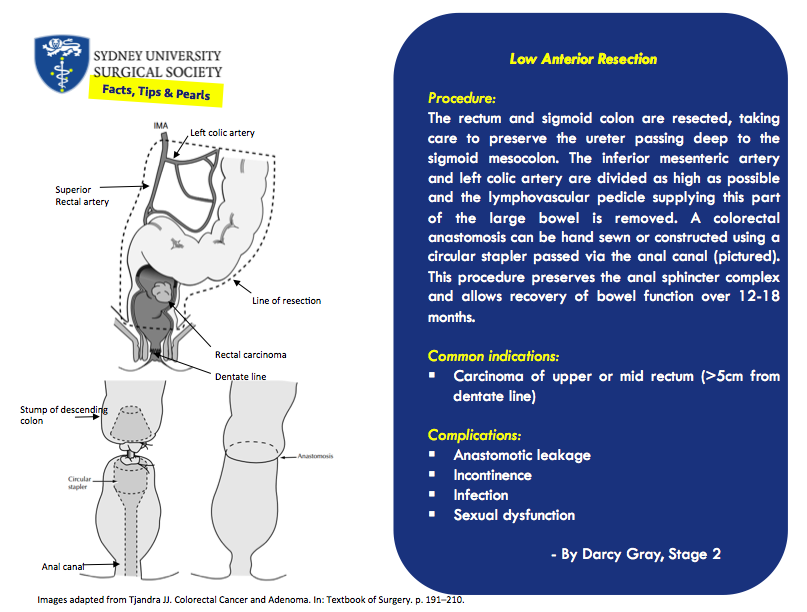
Low Anterior Resection
By Darcy Gray, Stage 2
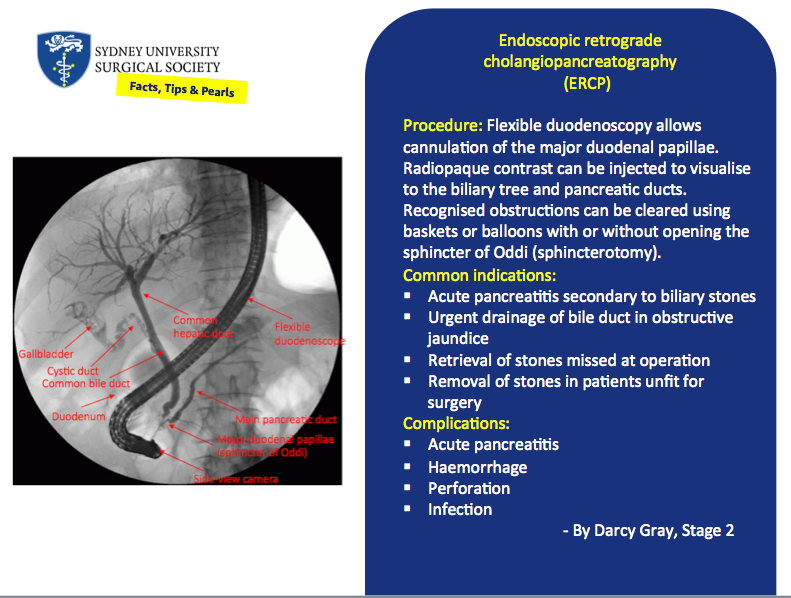
Endoscopic retrograde cholangiopancreatography (ERCP)
By Darcy Gray, Stage 2
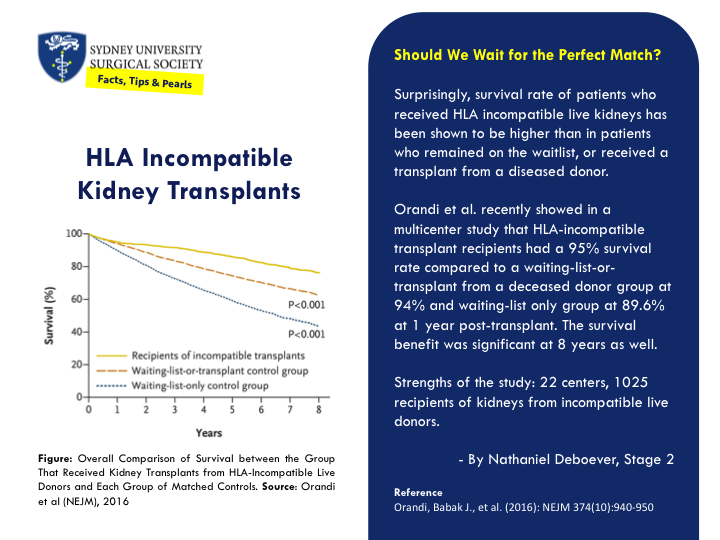
HLA-Incompatible Kidney Transplants
By Nathaniel Deboever, Stage 2
Neurosurgical ‘patties’
By Leonora Long, Stage 2
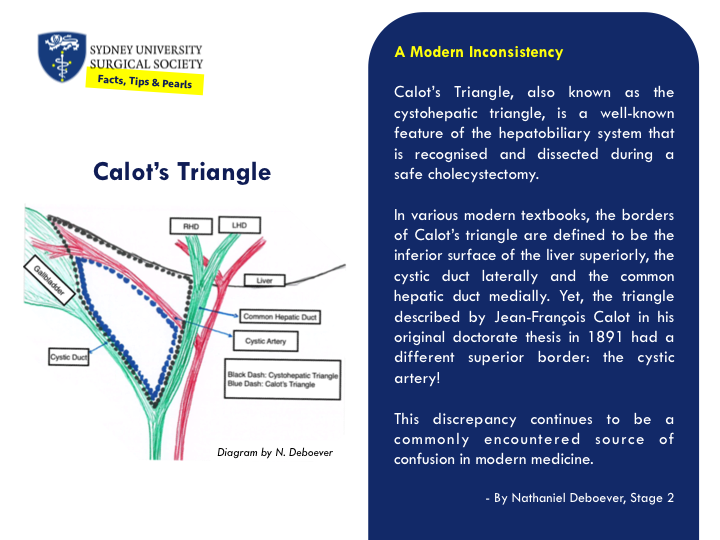
Calot’s Triangle: A Modern Inconsistency
Surgical Instruments
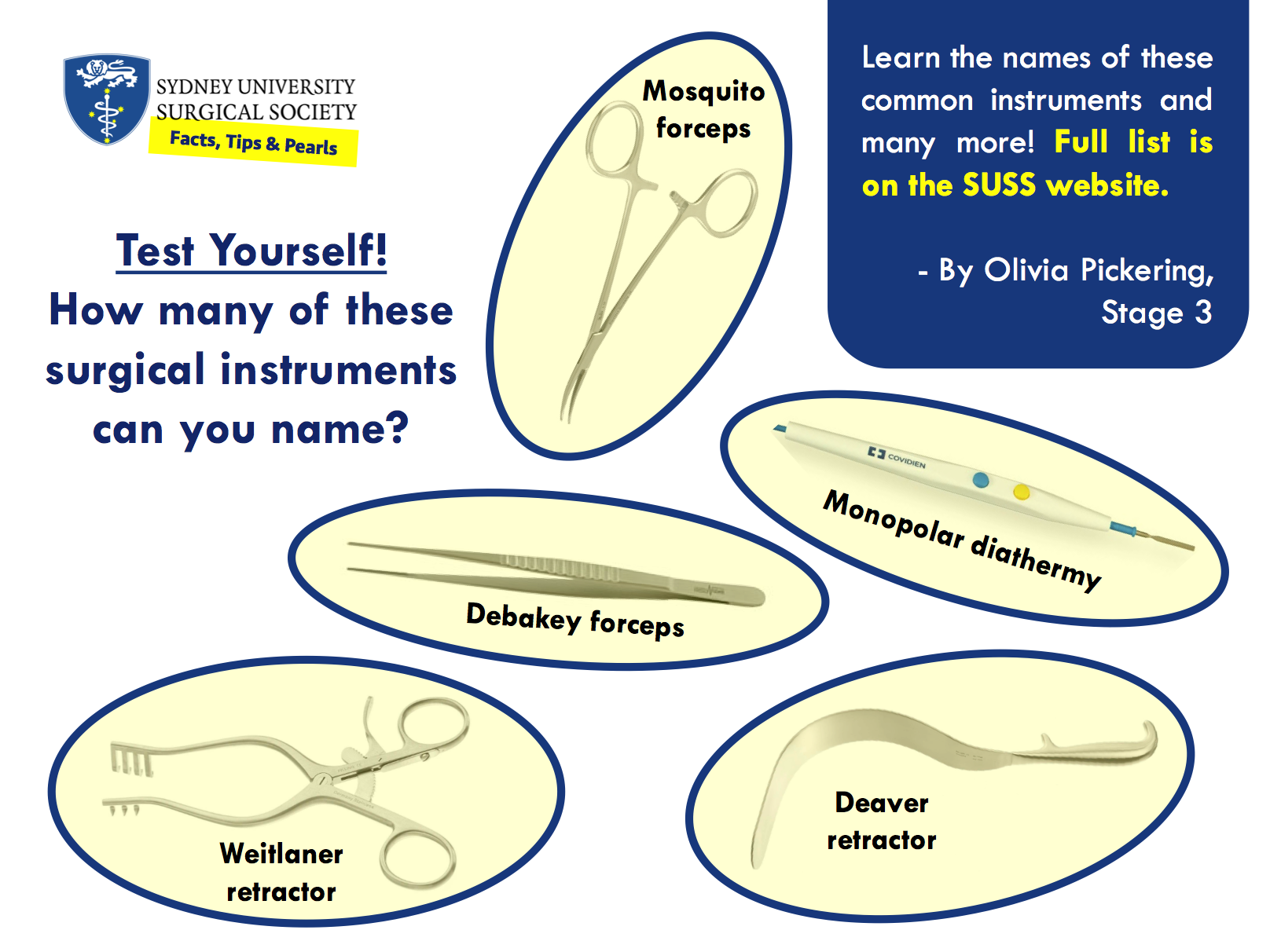
Instruments for Cutting
Forceps
Suction
Retractors
Electrosurgical Instruments
ENT and head and neck surgeon Dr Eric Levi
Dr Eric Levi on his favourite operations, future challenges for surgery, and social media in medicine.
by Alon Taylor
Alon Taylor: Who are you and what do you do?
Dr Eric Levi: My name is Eric and I’m an ear nose and throat, head and neck surgeon. I did my medical schooling and surgical training in Melbourne. Right now, I’m in Canada on my first of three fellowship years, currently subspecialising in head and neck surgical oncology, facial plastic and reconstructive surgery. The next two years will be in other countries in different subspecialty ENT areas.
AT: How did you settle on ENT surgery?
Dr EL: I suppose it’s through a process of discovery. Let me say this at the outset: I am a doctor first and a surgeon second. Every specialty within medicine and surgery is fascinating, interesting, and noble. There is not one specialty that is better than another. However, it is true that there are probably a few specialties that are better suited to you. As a medical student I was fascinated by emergency medicine, then neurology, then paediatrics, then obstetrics. But the more surgical rotations I did, and the more I studied surgery, the more I was drawn to it. It was at internship that I made up my mind to do surgery. I reserved my decision till then because I wanted to taste the life as a surgical intern and see first-hand the life of a surgical registrar and a surgeon. What you see as a medical student is different to what you actually see as a working doctor. The romantic notions of surgery you hear as a student are quickly offset by the realities of working in a high-pressure surgical unit day in and day out from 6 am to 8 pm with very few breaks. Once I made up my mind to do surgery, the choice of which surgical specialty was a little easier. I got to be a resident in almost all of the surgical specialties during basic surgical training and tasted the good and bad of each. I fell in love with ENT and its community of surgeons. I felt that ENT was the one specialty that suited me most.
AT: Best and worst parts of your job?
Dr EL: Other than earwax and tinnitus, the worst part of my job (and I think most surgeons would agree) is the demand for a total commitment of time, effort and intellect. Surgery is like an all or nothing phenomena. It demands all of you. The arduous training, the long hours, the physical expectation, the intellectual stamina and the emotional resilience required to be a surgeon is not to be taken lightly. When I do my 12-hour-long cases, I have to block out everything else and focus on that patient. When I’m on call, I need to be able to get up at 3 am, drive to the hospital and know that I can safely do a procedure. You don’t do shiftwork. You’re on almost all the time. Your patients expect a lot from you. Other clinicians expect a lot from you and the public demands a lot from you.
On the flip side, that demanding aspect of surgery is also the best part of my job. Some of us thrive under stress. We enjoy challenges. I get a real kick out of doing complex procedures, or just out of doing simple procedures well. I love my patients and I love learning about my patients in clinic, but if you were to push me hard I’d have to confess that I’m a surgeon simply because I really love surgical challenges and surgical problem-solving. There are some problems that can be fixed through expert craftsmanship. And that’s the best and most satisfying part of my job: a tangible difference in the lives of the patients I operate on.
AT: What is your favourite operation to perform and why?
Dr EL: In answering that question, let me also mention that actual surgery forms only a part of what we do as surgeons. The bigger part of surgery happens outside the operating room. There are a lot of non-surgical things we do as surgeons. So, my favourite operation would be my next one. I love the variety of procedures that ENT offers me. I remember the tracheostomy I did on a premature neonate that weighed a little heavier than my MacBook Pro. I remember fondly the cochlear implants on children and adults. I love the total nasal reconstruction. I also love the skullbase tumour resection, the craniofacial resection, the transphenoid pituitary, the acoustic neuroma, the orbital decompression, the jaw-neck resection, laser pharyngectomy, vocal cord injection, orbital exenteration, maxillectomy, carotid body tumour, dacrocystorhinostomy, laryngopharyngectomy, uvulopalatopharyngoplasty, stapedectomy, ossiculoplasty, rhinoplasty, blepharoplasty, local flaps, free flaps. Also the thyroids, parotids, tonsils, grommets, endoscopic sinus surgery and everything else in between. You just got me started there. Sorry.
AT: What were the challenges you faced on the path to where you are today?
Dr EL: I learned that I needed to accept rejection and that I can’t have it all. I knew that the training was demanding and arduous but I didn’t quite realise how hard it was until I was in it. Feel free to call me if you wanted to hear how many times I failed the job application, the interview, the selection, the exams, the research proposals, the manuscript submission, etc. Accepting rejection has become a normal part of surgical training for me. I also learned that I can’t be everything I wanted to be: husband, dad, traveller, social animal, party goer and surgical trainee all at the same time. Something’s gotta give. I couldn’t go to all the holidays, concerts, and parties that I wanted. I had to miss out on some of my wife and kids’ significant moments due to exams, conferences, emergency cases and the like. Thankfully, I don’t do surgery alone. I am where I am today because of the support of my loved ones. Now that I am a fellow and a consultant, it gets a little easier as I have a slightly better control of my days. It still requires a huge effort to maintain work-life harmony though. A constant evolving challenge. A worthwhile challenge. One of the simple philosophies of life I hang on to is this: if you love your work, good work will come to you. Love what you do (no matter how challenging it is) and then you will get to do what you love.
AT: What do you see as the major issues facing surgery today?
Dr EL: There have always been and there will always be many issues facing surgery because of the reality of the world we live in. Some major issues include bullying, harassment, gender equality, work safety, resource allocation, surgical selection, training competence, ethical responsibility, global surgery, etc. Many other experts can speak directly and with greater depth about those issues. Some may disagree with this, but in my opinion, the biggest challenge affecting surgeons individually and as a profession is the problem of surgery losing its clinical heart. Surgeons are increasingly reduced to mere proceduralists and technicians. Clinical decisions are being taken away from surgeons and restrictions are imposed upon what we do by non-clinicians. Everything from procedure duration, operating costs and length of stay are measured as if surgeons and patients were indistinguishable factory line products. The long-term effect of this is that surgeons will be seen as skilled but uneducated technicians. This will be unfortunate because there’s so much clinical wisdom and expertise outside the operating theatre that is required to be a good surgeon. Performing an operation is only a part of surgical competence. Why the operation, getting the diagnosis right in the first place, when, where, which technique, what to do, what not to do, when not to do the operation, what happens before and after the operation, rehabilitation after the operation – those are even more significant surgical competencies. That kind of surgical wisdom comes from knowing the heart and essence of surgery: that surgeons are first of all doctors, but doctors who happen to also be trained in the use of the scalpel.
AT: What advice would you give to medical students with a budding interest in surgery?
Dr EL: Very few of us know that we are born to be a cardiac transplant surgeon, paediatric spinal surgeon or epilepsy surgeon. For the rest of us, keep your options open. Don’t be infatuated by media descriptions of surgery. Don’t eliminate options too early. Taste the life of surgery before fully committing to it. It’s a costly journey financially, physically, emotionally, socially. Make sure you’re willing to pay the price. Decide firstly if you want to be a surgeon at all. Once you decide on surgery, think about what problems you like solving. Don’t focus on the operations themselves. Think about what kinds of problems excite you. If possible, get a feel of the specialty community. Is there much collegiality in that specialty? Will you like the people you will be working with for the next 30 years?
AT: You are very active on social media. What do you see as the importance of social media for a clinician?
Dr EL: Now this question deserves a whole lecture, seminar and textbook in itself. I won’t go into too much detail as I and many others have written extensively on Social Media in Medicine elsewhere, but I will say this: I’m on social media because my patients and trainees are already there. I need to understand what kinds of information are being fed to my patients. I need to understand the current challenges facing my trainees. Social media helps me to listen in on these conversations. Once in a while I get the privilege of helping others through social media in the form of education and engagement. That’s nice, and it goes back to the essence of our roles as doctors. We are teachers and helpers. We sometimes get invited to engage with others and help them lead better lives.
Five minutes with a female general surgical trainee